EN
Translate:
EN
Signed in as:
filler@godaddy.com
EN
Translate:
EN
Signed in as:
filler@godaddy.com

The macula or macula lutea (“yellow spot” in Latin) is an oval yellow area near the center of the retina of the human eye.
At the center of the macula is the fovea: with the largest concentration of cone cells (responsible for detailed vision and colour vision) in the eye and is responsible for central vision. Within the macula is the fovea – a small depression in the macula – which contains a high density of cones (photoreceptors with high acuity).
The macula has an important and naturally occurring protective substance known as the macular pigment (MP) • 黃斑色素 . The MP is made up of several carotenoids (phytochemicals – found in plants) commonly found in certain fruits and vegetables that provide the red, orange and yellow colors of these foods. The MP is made of three known compounds:
Lutein and Zeaxanthin are obtained through food and are found primarily in broccoli, corn, squash and dark green leafy vegetables like spinach and kale. Meso-Zeaxanthin is obtained by an enzyme conversion of Lutein to Meso-Zeaxanthin in the macula. A recent peer reviewed study published, August of 2014, in Journal of Food Processing & Technology has verified the presence of MZ in salmon skin, sardine skin, trout skin and trout flesh. This study confirmed the presence MZ in nature, and in the human food chain.
In a 1994 Journal of American Medical Association report, Dr. Johanna M. Seddon and her associates at Harvard University found that 6 mg per day of lutein lead to a 43 percent lower risk for Macular Degeneration.
“When we compared the amount of macular pigment, which is comprised of Lutein and Zeaxanthin, present in the eyes of people with age-related macular degeneration to people without the disease, those with the lowest levels of carotenoid accumulation in the outer retina were significantly more likely to suffer from age-related macular degeneration than those with higher pigment levels, ” said Dr. Landrum. “The difference in risk between those having the highest and lowest levels was 75 percent.”
2003, Vrabec, Tantri et al. Autosomal dominant Stargardt-like macular dystrophy: identification of a new family with a mutation in the ELOVL4 gene. Am J Ophthalmology
Lutein and Zeaxanthin are dietary carotenoids (pigments) that filter damaging high energy blue wavelength light from the visible-light spectrum by as much as 90%. Lutein and Zeaxanthin are also antioxidants and therefore protect against the damage caused by harmful molecules that are produced through normal body processes, such as oxygen metabolism, these are called free radicals. Environmental sources of free radicals include cigarette smoke, air pollutants, radiation, certain drugs and environmental toxins.
Meso-Zeaxanthin, 中玉米黃素, the most potent antioxidant of the three carotenoids, is only found in the center portion of the macula where vision is sharpest. Meso-Zeaxanthin is obtained converting ingested Lutein inside the retina and is not found in the diet. Most Macular Degeneration patients have 30% less Meso-Zeaxanthin in their macula* and show an inability to convert Lutein into Meso-Zeaxanthin. Supplementation with MacuHealth with LMZ3 will ensure that this crucial component of macular pigment accumulates in the target tissue (i.e. the central macula) in a way that is not dependent on an enzyme converting Lutein to Meso-Zeaxanthin.
Source: https://www.macuhealth.com/learning-center/macular-pigment-density/
Lutein • Zeaxanthin • Meso-Zeaxanthan 10•2•10mg
葉黃素 • 玉米黃素 • 中玉米黃素
Vision Essence Early Defence® is a triple-carotenoid ocular nutrition formula containing all three macular protective pigments, providing antioxidants for the maintenance of eye health. Taken once daily to increase macular pigment density, Vision Essence Early Defence helps maintain eyesight in conditions associated with sunlight damage, such as cataracts and age-related macular degeneration (AMD).
Eye care professionals advise increasing intake of macular pigments to protect and improve eyesight at the first signs or concerns of retinal disease, including early AMD, diabetic eyes, and family history of AMD. Helps maintain visual performance in healthy eyes.
Why is meso-zeaxanthin important in the Vision Essence formulas?
Supplementation trials with lutein, alone, have shown only modest results in increasing macular pigment volume (MPD). Studies which included meso-zeaxanthin demonstrated more rapid and robust increases in MPD. (Ma, 2016)

Lutein, Zeaxanthin and Meso-zeaxanthin Supplementation Associated with Macular Pigment Optical Density.
FINDINGS
Our results showed that the carotenoids supplementation significantly increased the level of Macular Pigment Optical Density and the inclusion of meso-zeaxanthin resulted in a greater increase in macular pigment compared to supplements lacking this central carotenoid.
Ma et al., 2016 Nutrients.
Zinc:
good for some, harmful for others.
For AMD patients with a specific genotype, the risk of developing wet AMD is tripled by taking supplemental zinc formulations (25 mg per day and higher), which increases the risk of vision loss.
Avoid high-dose zinc if:
· you have early stage age-related macular degeneration (AMD)
· you've not undertaken AMD genetic testing cheek swab
Common drug store "eye vitamins" contain mega-doses of zinc (>25mg), accelerating AMD through the early stages, and for those with a common genetic profile, about 1 in 6 individuals.
Our eye doctors will help you navigate the risks and obtain the right ocular nutrition formula.
A genetic test to determine zinc compatibility is strongly advised.
Source: Vision Essence

OUR SOLUTIONS
Specialized formula to improve sight and protect vision in the face of retinal diseases
Vision Essence Early Defence®
is a triple-carotenoid ocular nutrition formula containing all three macular protective pigments, providing antioxidants for the maintenance of eye health.
Taken once daily to increase macular pigment density, Vision Essence Early Defence helps maintain eyesight in conditions associated with sunlight damage, such as cataracts and age-related macular degeneration (AMD). Eye care professionals advise increasing intake of macular pigments to protect and improve eyesight at the first signs or concerns of retinal disease, including early AMD, diabetic eyes, and family history of AMD.*
Helps maintain visual performance in healthy eyes.
Vision Essence Zinc-free3+MZ
alternative to the U.S. NEI-NIH formula- contains no zinc or beta-carotene. It combines all three macular protective pigments with vitamins C and E to provide antioxidants for the maintenance of eye health.
Two capsules taken daily increases macular pigment density to help maintain eyesight in conditions related to sunlight damage, such as age-related macular degeneration (AMD). Vision Essence Zinc-free3+MZ is advised for those sensitive to high-dose zinc supplements, and those who’ve not performed genetic testing to determine if zinc supplements will accelerate AMD.
This formula is not advised for early stage AMD.
Recommended for: Patients with intermediate stage / category 3 AMD who've not completed the VitaRisk genetic test, or the test advises zinc avoidance.
Vision Essence GTG3-Low-Zinc+MZ
alternative to the U.S. NEI-NIH formula- contains no beta-carotene. It combines all three macular protective pigments with a reduced dose of zinc and vitamins C and E to provide antioxidants for the maintenance of eye health.
Two capsules taken daily increases macular pigment density to help maintain eyesight in conditions related to sunlight damage, such as age-related macular degeneration (AMD). Vision Essence Zinc-free3+MZ is advised for those sensitive to high-dose zinc supplements, and those who’ve not performed genetic testing to determine if zinc supplements will accelerate AMD.
Formulas containing zinc are not advised for early stage AMD.
For AMD patients with a specific genotype, the risk of developing wet AMD is tripled by taking supplemental zinc formulations (25 mg per day and higher), which increases the risk of vision loss.
A genetic test to determine zinc compatibility
is strongly advised.

Why use Early Defence® for diabetic eyes?
Similar to AMD, the diabetic retina
can be characterized by:
· low macular pigment density and poor contrast sensitivity
· elevated inflammatory markers and impaired innate anti-oxidative/anti-inflammatory capacity (TNF, CRP, CFH, SOD2, NRF2)
· mitochondrial dysfunction
· tissue ischemia, hypoxia, and oxidative stress
· upregulation of vascular endothelial growth factor (VEGF), & choroidal neovascularization (CNV) - also termed Proliferative Diabetic Choroidopathy. (Hua et al., 2017)
Increasing the Macular Pigment Density in diabetic eyes is known to improve visual function. (Hu, 2016) (Garcia-Medina, 2016) (Roig-Revert, 2015) (Moschos, 2017)
Vision Essence Early Defense® is formulated with all three macular protective pigments known to increase macular pigment volume.

WHAT IS AMD?
AMD, Age-related Macular Degeneration, is a progressive eye disease affecting the clear central vision needed for daily activities like reading or driving, leaving only peripheral vision intact. As toxic drusen deposits build up in the macula, cells responsible for vision begin to break down under oxidative attack, leading to poor visual function. 1 in 5 AMD cases develop into the advanced form.
A diagnosis of AMD can be scary
Fortunately, AMD is generally a slow moving condition, and most people have an early form. This buys time to make positive lifestyle changes such as improving diet, exercise habits, and adding ocular nutrition products to help maintain eyesight.
AMD GENETIC TESTING
If you have intermediate stage AMD, a genetic test will help determine an individualized follow-up schedule based on genetic risk to closely monitor your condition.
Zinc, which is commonly found in ocular nutrition products, may be helpful or harmful. This can only be determined by your DNA*.
2012_Improvement of Retinal Function in Early Age-Related Macular Degeneration After Lutein and Zeaxanthin Supplementation: A Randomized, Double-Masked, Placebo-Controlled Trial. AJO, American Journal of Ophthalmology

The Nation Eye Institute (NEI) and American Academy of Ophthalmology (AAO) Preferred Practice Pattern Guidelines advise against the AREDS formulas for early stage AMD.
AREDS Report #8 indicated potential harm from zinc use by early AMD patients. (Chew, 2001)
Some individuals will experience harmful results from taking zinc due to a common AMD genetic risk profile.
Only the VitaRisk genetic test can identify people who should avoid high-dose zinc supplements. (Kaufman, 2020) (Vavvas, 2018) (Seddon, 2016) (Awh, 2014, 2013)
The best choice for early stage retinal conditions is a macular pigment carotenoid formula containing lutein, zeaxanthin, and meso-zeaxanthin.
葉黃素 • 玉米黃素 • 中玉米黃素
Source: Vision Essence
Macular Pigment Supplementation: A Prescription for Vision & Cognitive Health - John Nolan, PhD

AMD is a common eye condition and a leading cause of vision loss among people age 50 and older.
It causes damage to the macula, a small spot near the center of the retina and the part of the eye needed for sharp, central vision, which lets us see objects that are straight ahead.
In some people, AMD advances so slowly that vision loss does not occur for a long time. In others, the disease progresses faster and may lead to a loss of vision in one or both eyes.
As AMD progresses, a blurred area near the center of vision is a common symptom. Over time, the blurred area may grow larger or you may develop blank spots in your central vision. Objects also may not appear to be as bright as they used to be.
AMD by itself does not lead to complete blindness, with no ability to see. However, the loss of central vision in AMD can interfere with simple everyday activities, such as the ability to see faces, drive, read, write, or do close work, such as cooking or fixing things around the house.
Even more devastating is the lost of independence, personal self confidence, plus the continuous monthly 2-4 hour eye check-ups and never ending monthly or bi-monthly intra-ocular eye injections of anti-VEGF medication to prevent or reduce the damage of macular hemorrhage that causes blindness.
The Macula
The macula is made up of millions of light-sensing cells that provide sharp, central vision. It is the most sensitive part of the retina, which is located at the back of the eye. When the macula is damaged, the center of your field of view may appear blurry, distorted, or dark.
In its early and intermediate forms, Dry AMD presents as small deposits on the retina comprised of cholesterol and complement (inflammatory) proteins called Drusen and pigmentation changes in the macula.
The advanced form may be dry geographic atrophy (30% of advanced disease) or wet choroidal neovascularization (70% of advanced disease).
In Wet AMD, abnormal blood vessels grow under the retina to aid nutrient transport to the macula
(choroidal neovascularization or CNV).
Reference: NEI, National Eye Institute, AMD Facts https://nei.nih.gov/health/maculardegen/armd_facts

As the leading cause of adult blindness in developed countries, age-related macular degeneration is three times more common than glaucoma and affects one in eight adults over age 60. Though common, it often goes undiagnosed until after significant, irreversible vision loss has occurred. Knowing the signs and symptoms of AMD is the first step toward preventing the dramatic consequences of untreated disease.
Some symptoms of macular degeneration are detected early, yet not connected to the disease until after the condition is fairly advanced. Other symptoms seem more obtrusive and are likely to trigger a visit to
the eye care professional:
A landmark study published recently in JAMA Ophthalmology shows at least
25% of clinical AMD is going undiagnosed
in primary eye care today.
Moreover,
30% of the undiagnosed patients had large drusen,
a known risk factor for advanced AMD (wet AMD).
Complementing structural exams with functional dark adaptation evaluation helps safeguard against failure to catch clinically-detectable AMD. Dark adaptation testing using AdaptDx provides a clear, objective measure that is easy to interpret.
2017, Neely, Bray , Prevalence of Undiagnosed Age-Related Macular Degeneration in Primary Eye Care. JAMA Ophthalmology
Cholesterol deposits accumulate in the macula years before drusen are visible, making drusen the tip of the iceberg in AMD pathology.
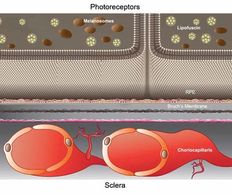
Before drusen are visible, an invisible layer of cholesterol builds up between the pigmented layer of the retina (RPE) and the elastic layer of Bruch’s membrane. These cholesterol deposits—basal laminar (BLamD) and basal linear (BLinD)—cause oxidative stress and inflammation, hindering nutrient transportation to photoreceptor cells.ii As photoreceptor cells die, it becomes harder for the eyes to adjust to darkness and night vision declines.
This Dark Adaptation™ impairment is the first sign of AMD.
Prior to pivotal research conducted at the University of Alabama Birmingham, the Alabama Study on Age-Related Macular Degeneration (ALSTAR), AMD was staged as early, intermediate, and advanced. Thanks to the groundbreaking findings of this investigation, we can identify a subclinical stage of AMD.
Reference: 2016, Owsley, McGwin, Clark, Delayed Rod-Mediated Dark Adaptation is a Functional Biomarker for Incident Early Age-Related Macular Degeneration (ALSTAR), Journal Ophthalmology.
Also known as “night blindness,” impaired dark adaptation is the earliest symptom of AMD. Physical changes occurring in the early development of AMD compromise the eye’s ability to adjust to darkness. This can make it difficult to drive at night, read in dim light or adjust to dark places, like walking into a dark movie theater. More noticeable visual deficits become evident as the disease progresses, such as worsened visual acuity, distorted vision and central vision loss.
Dark Adaptation impartment will occur many years before any visible structural changes are detectable in your eye by your doctor.
Dark adaptation testing utilizing AdaptDx, provides a clear, objective measure that is easy to interpret.
Structural changes (the appearance of drusen) in the retina are not always easily discernible. They often become evident only after AMD has progressed from a subclinical state.
But AdaptDx® is 90% sensitive and 90% specific in identifying the earliest onset of AMD. This makes AdaptDx more accurate than current testing for glaucoma (as the accuracy of visual field is only 83%).
Being able to detect AMD with such accuracy will greatly improve your patients’ outcomes. It allows you to detect AMD at the earliest stage, at least three years before drusen are visible, when action can be taken to slow disease progression and prevent vision loss.
.
.

From subclinical to advanced AMD, all stages of the disease are the manifestation of the same underlying pathology
Diagnosing the earliest stages of AMD can present a challenge because these patients often have good corrected visual acuity and the retina appears normal upon clinical examination. Consequently, a routine vision test may not raise any suspicion of the disease.
Subtle yet progressive, night vision difficulty is the earliest symptom of AMD. Often presented as problems driving or reading at night, impaired Dark Adaptation function is the first biomarker of AMD—with impairment taking place at a subclinical level at least three years before drusen are visible.
No pigmentary abnormalities are apparent upon examination at this stage, and if drusen is detected, these are <63 μm.
Most people do not experience vision loss in the early stage of AMD, but night vision problems are often reported. Though no pigmentary abnormalities are apparent upon examination, medium-sized drusen (>63 μm and ≤125 μm) are present.
At this stage, some people may see a blurred spot in the center of their vision. In addition to night vision issues, these patients may also have issues with contrast sensitivity. Some pigmentary abnormalities may be observed and at least one druse >125 μm is present.
· Choroidal Neovascularization (CNV) or “Wet AMD” occurs in about 10-15% of patients as a result of abnormal blood vessels forming under the central retina. Vision distortion and/or vision loss begins when these blood vessels leak into the retina. Vision loss caused by Wet AMD typically occurs quite rapidly. However, if the wet form is caught early enough, treatment by a retinal specialist can stabilize vision.
· Geographic Atrophy (GA) or “Advanced Dry AMD” is an advanced form of AMD, during which cells within a region of the retina waste away and die (atrophy). These regions of cell atrophy result in a blind spot in the visual field that cannot be reversed.
Reference: 2016, Owsley, McGwin, Clark, Delayed Rod-Mediated Dark Adaptation is a Functional Biomarker for Incident Early Age-Related Macular Degeneration (ALSTAR), Journal Ophthalmology.

Personalized Treatment for AMD Using Genetics
Peer Reviewed Science :
Scientific studies as recent as 2018 and 2019 serve as clear evidence of the relationship between a specific genetic group and long-term use of zinc (such as the AREDS formulations), which increase progression of the disease to wet AMD (nvAMD) in patients with dry AMD. This recent research is built upon years of prior scientific genetic discoveries in AMD.
The largest and most complete validation of the clinical utility of the Vita Risk Test was performed by an international group of investigators led by Dr. Demetrios Vavvas MD (Harvard University and the Massachusetts Eye and Ear Infirmary), which showed that 15% of patients carried a genetic profile that increased progression to wet AMD after chronic exposure to zinc.
This genetic profile is defined as 2 complement factor H risk variants combined with an absence of risk markers at the ARMS2 locus. These are the two major genes associated with AMD risk.
These patients had almost three times the risk of progression to nvAMD, wet macular degeneration compared to those not receiving supplements.
Understanding your unique AMD genetic profile could help your doctor guide you to the right supplement options, ensuring you are not harmed by the zinc in most eye supplements.
Our eye doctors will help you navigate the risks with a simple cheek swab test, the Vita Risk or Macula Risk Genetic Test to provide this information.
Genetic research reveals that zinc-based eye vitamins in the AREDS/AREDS2 Age-related Eye Disease Studies used to prevent the progression of age-related macular degeneration (AMD) are not safe for 15% of patients.
For AMD patients with a specific genotype,
the risk of developing wet AMD is tripled by taking supplemental zinc formulations (25 mg per day and higher), which increases the risk of vision loss.
Avoid high-dose zinc if:
Common drug store "eye vitamins" contain mega-doses of zinc, accelerating AMD through the early stages, and for those with a common genetic profile, about 1 in 6 individuals.
Dr Jerome Sherman discusses the importance of genetic testing and the value customized AMD vitamin supplementation based on your genome type.
While we try to inform you of your OHIP eligibility before your eye exam, we are only able to assess your final eligibility for OHIP after your doctor has examined your eyes.
Masks are still required for your visit as per the guidelines from Ministry of Health
i-Blog: April 8 Solar Eclipse Safety 日食安全
Myopia Control Information 近視控制資訊
雖然我們會在你進行眼科檢查之前告知你符不符合OHIP檢查的資格,但我們只能夠在你的醫生進行眼睛檢查後才能夠知道你符不符合OHIP檢查的資格。
根據安省衛生廳提供最新的的指引,你仍然需要佩戴口罩。